Residual MACE in CAD: What Are the Long-Term Adverse Cardiac Events to Worry About?
Uwe Zeymer, MD
Symptomatic coronary artery disease (CAD) affects over 150 million patients worldwide and is caused when atherosclerotic plaques form in the coronary arteries, limiting blood flow to the heart. The rupture of one of these plaques can lead to the formation of a blood clot, which partially or completely blocks blood flow, leading to an acute myocardial infarction (MI). Because atherosclerosis very often develops systemically, patients with CAD often have plaques in the lower limb arteries or the carotid arteries as well. CAD is therefore frequently associated with a variety of ischaemic events, such as stroke and ischaemic events in the legs.
Most clinical trials in this therapy area measure the composite endpoint of major adverse cardiovascular events (MACE), the combination of MI, stroke or death from cardiovascular causes. MACE are the most severe atherothrombotic events, and the most feared by patients because of their high risk of mortality or irreversible harm. Unfortunately, they are also relatively common – in the REACH registry, MACE affected nearly 1 in 20 patients with CAD over a 1-year timeframe. This risk is even greater in certain types of patients, such as those with polyvascular disease or those with co-morbidities such as heart failure or diabetes (Table). Patients with chronic kidney disease alongside CAD are also at a higher risk of MACE, compounded by the fact that they often do not receive the same medications offered to patients with normal renal function. With multiple risk factors (e.g. co-morbidities or older age), the risk of MACE increases still further (Figure 1).
Table. Selected high-risk subgroups based on data from the REACH registry.
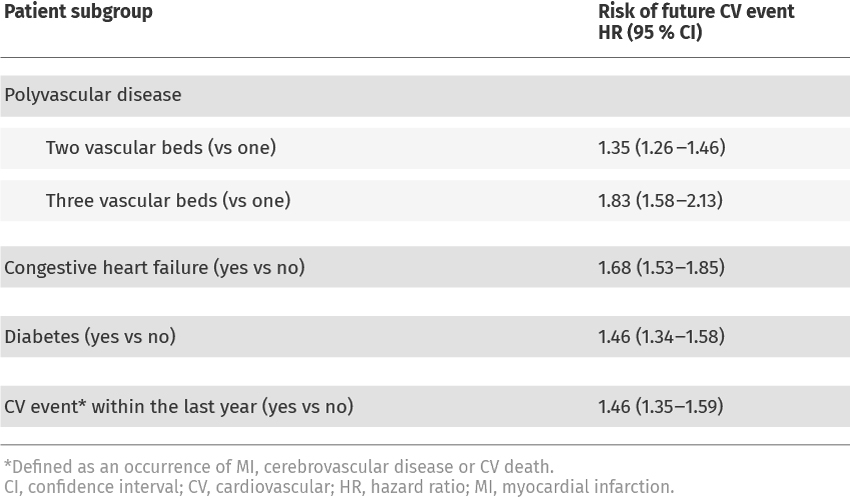

Figure 1. Cumulative rate of MACE-free survival after an MI according to the number of risk factors (age >65 years, diabetes, second MI, GFR <60 ml/min, multi-vessel CAD).
CAD, coronary artery disease; GFR, glomerular filtration rate; MACE, major adverse cardiovascular events; MI, myocardial infarction.
As well as posing a high risk of death or permanent disability, both MI and stroke are associated with a high risk of recurrence – in one UK-based study, roughly one-quarter of all ischaemic strokes and MIs were recurrent events. This is supported by data from the large international REACH registry, which showed that patients with a previous ischaemic event were 40–70% more likely to experience a MACE than patients with no previous event (Figure 2). In patients with CAD and a previous stroke or transient ischaemic attack, the risk of MACE was as high as 25% over 4 years – approximately 50% higher than in patients with no history of cerebrovascular events.

Figure 2. Risk of MACE according to previous ischaemic events in the REACH registry
CV, cardiovascular; MACE, major adverse cardiovascular events; MI, myocardial infarction.
In order to reduce the risk of MACE, clinical guidelines from the European Society for Cardiology (ESC) recommend that patients with CAD should receive a comprehensive programme of risk factor management and antithrombotic therapy. This includes therapies to reduce plaque formation by reducing blood lipid levels and managing high blood pressure, as well as an antiplatelet (usually aspirin) to reduce clot formation. Despite these approaches, approximately 10% of patients with vascular disease still experience MACE over a 2-year period, highlighting the need for improved management strategies for these high-risk patients.







