EHRA 2022 Congress Highlights
Congress summary
The annual European Heart Rhythm Association (EHRA) congress took place on 3–5 April 2022, with delegates attending both virtually and in-person once again in Copenhagen, Denmark. Atrial fibrillation (AF) is the most prevalent sustained cardiac arrythmia in the world1 and, as such, was a main topic of discussion in the scientific programme of EHRA, the leading network of European cardiac rhythm management specialists.
The Bayer-sponsored symposium, ‘What if? Protecting your patients from stroke, no matter their journey’, is available to view on demand. The symposium followed a fictional 72-year-old patient with diabetes and AF, Julia, and considered how she could be protected from stroke in various clinical scenarios.
You can also listen to a follow-up podcast featuring Professor John Camm (London, UK) and Professor Keith Fox (Edinburgh, UK) who discuss the management of patients with AF undergoing percutaneous coronary intervention (PCI) in more depth.

Simple and practical care pathways for patients with AF
Since 2020, the European Society of Cardiology (ESC) and European Association for Cardio-Thoracic Surgery (EACTS) have encouraged a simple, holistic approach to patient management - the Atrial fibrillation Better Care (ABC) pathway.1 This remained a central theme in discussions on the treatment of AF throughout the congress.
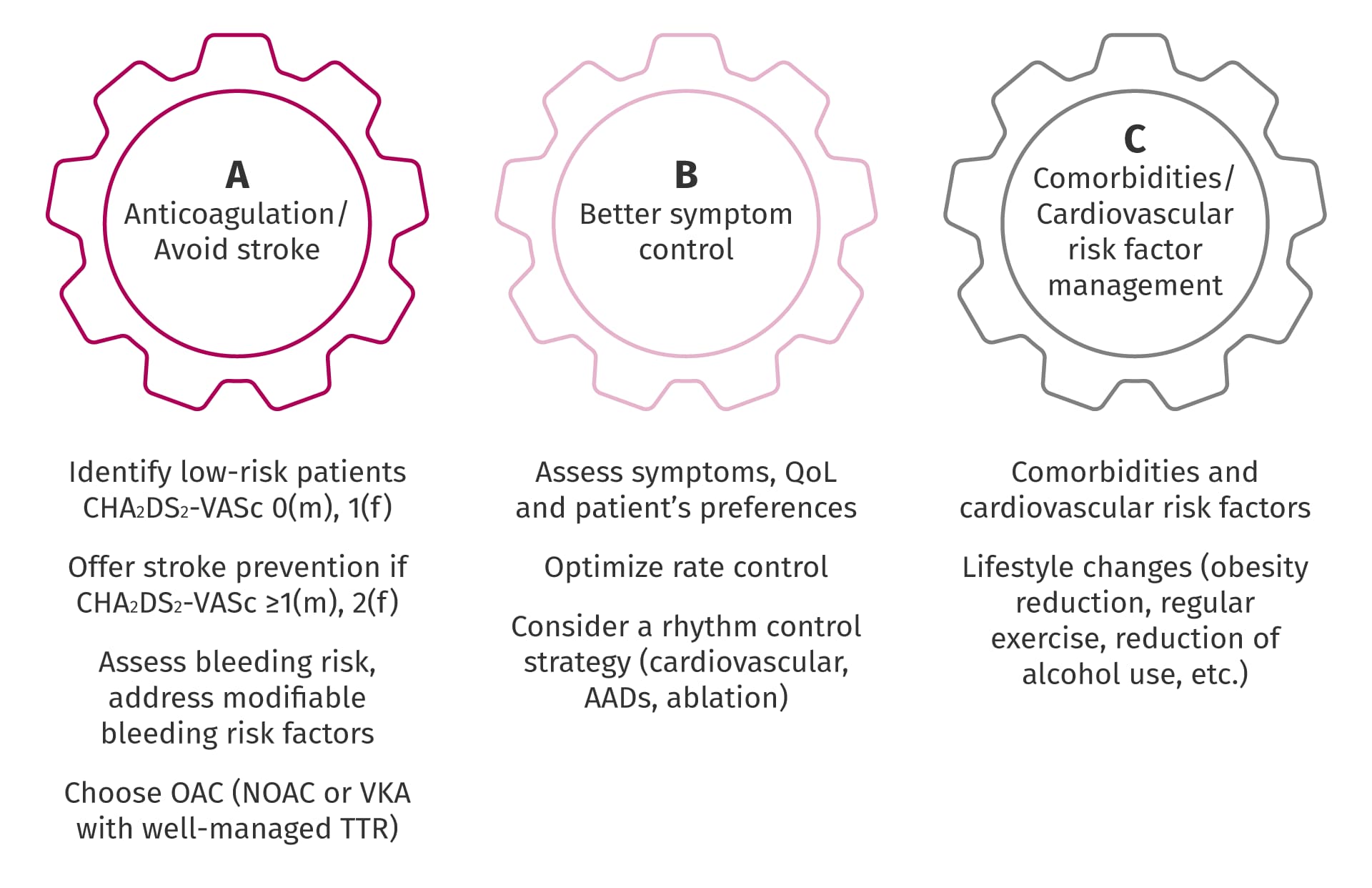
Treat AF: The ABC pathway1
AAD, anti-arrhythmia drug; AF, atrial fibrillation; CHA2DS2-VASc, Congestive heart failure, Hypertension, Age ≥75 years (2 points), Diabetes mellitus, Stroke or transient ischaemic attack (2 points), Vascular disease, Age 65–74, Sex category (female); NOAC, non-vitamin K antagonist oral anticoagulant; OAC, oral anticoagulant; QoL, quality of life; TTR, time in therapeutic range; VKA, vitamin K antagonist.
The first step of the ABC pathway was explored by Dr Emma Svennberg (Stockholm, Sweden) during the Bayer-sponsored symposium. Dr Svennberg discussed the Swedish multicentre randomized controlled trial STROKESTOP, which investigated whether screening patients aged 75–76 years for AF with a single-lead electrocardiogram could identify AF and prevent adverse outcomes. The study found a significant 4% relative risk reduction and 1.1% absolute risk reduction of the primary endpoint in patients randomized to screening versus those that were not screened. This demonstrates how early detection and awareness of your patients’ AF can help enable timely initiation of oral anticoagulation treatment, which can help to safeguard them from potentially devastating thromboembolic outcomes.2

Incidence of the combined primary endpoint of ischaemic or haemorrhagic stroke, systemic embolism, all-cause mortality, or hospitalization for bleeding in the STROKESTOP study2
CI, confidence interval; HR, hazard ratio.
Considering co-morbidities in patients with AF
While many sessions in the congress focused on the second step of the ABC pathway, better symptom and rhythm control, the final step of the ABC pathway, the management of comorbidities and cardiovascular risk factors, was the main focus of the Bayer-sponsored symposium.

The symposium panel discussing the protection of Julia, a fictional patient with AF, in various clinical scenarios
AF, atrial fibrillation; CKD, chronic kidney disease; EHRA, European Heart Rhythm Association; NVAF, non-valvular atrial fibrillation; PCI, percutaneous coronary intervention
Professor Keith Fox considered the additional care required if Julia underwent an elective PCI, noting that patients with AF and coronary artery disease present a therapeutic challenge with regard to anticoagulation. During an interview following the symposium, Professor Fox stated that ‘patients with AF have a double jeopardy because they have, in many instances, underlying coronary artery disease and we need to address both the requirements of stroke prevention and also minimization of the risks of stent thrombosis. So, both have to be addressed while also minimizing bleeding risks.’
The benefit of dual therapy compared with triple therapy in patients with AF undergoing PCI was explained by Professor Fox, who presented data from both the PIONEER AF-PCI randomized controlled trial and the real-world RIVA-PCI study.3,4 This benefit has been reflected in the 2020 ESC guidelines on the management of acute coronary syndromes, which have moved away from recommendations for prolonged triple therapy and towards the use of dual therapy and non‑vitamin K antagonist oral anticoagulant (NOAC) monotherapy in patients with AF undergoing elective PCI.*5
*Guidelines may vary by region. Please refer to your local guidelines for details.

Adverse outcomes in patients with AF undergoing PCI receiving have been shown to be consistently low in both RCTs and real-world studies3,4
These results are not intended for direct comparison. Different study designs, populations and study/treatment durations. *Rivaroxaban 15 mg od plus a P2Y12 inhibitor (n=694 for efficacy endpoints, n=696 for safety endpoint). 12-month follow-up. #Registry data; dosing information not available. Graph shows results of 448 patients treated with rivaroxaban for >9 months during a 14-month follow-up. Follow-up rate 92.9%.
AF, atrial fibrillation; CV, cardiovascular; ISTH, International Society on Thrombosis and Haemostasis; MI, myocardial infarction; od, once daily; PCI, percutaneous coronary intervention; RCT, randomized controlled trial.
Additional considerations for the management of patients with AF undergoing elective PCI
Listen to Professor John Camm and Professor Keith Fox expand on why patients with AF undergoing PCI need such close attention when choosing an antithrombotic regimen. They also provide their perspectives on how patients with AF undergoing catheter ablation can be best protected from cardioembolic stroke.
‘Achieving the right balance between the risk of bleeding and thrombosis is important and often difficult but made much easier by the availability of non-vitamin K oral anticoagulants.’
Professor John Camm
Professor Potpara (Belgrade, Serbia) focused on an additional challenge often faced by patients with AF: chronic kidney disease. She outlined the breadth and depth of evidence for the benefit of NOAC treatment in patients with AF and co-morbid chronic kidney disease and diabetes over vitamin K antagonists.
Following a question posed during the question and answer session, Professor Potpara highlighted how multidisciplinary teamwork is key in identifying and managing risk factors contributing to stroke risk in patients with AF. The importance of collaboration was reiterated by Professor Gregory Lip (Liverpool, UK) during a session on shared decision making in a persistent AF patient. Professor Lip discussed that patients with AF often present in various clinical settings and therefore a consistent approach to their care and management is required.
The role of the patient in successful stroke prevention
The final presentation in the Bayer-sponsored symposium was delivered by former EHRA president Professor John Camm. Professor Camm demonstrated that NOACs have been proven to provide consistent protection as your patients get older and explored how you can support them to adhere to their treatment regimen. He expanded on this in an interview following the symposium, in which he noted that ‘in order to improve adherence, we must talk to the patient… they have to understand that they’re taking [medication] to prevent a severe consequence of atrial fibrillation, stroke. Nobody wants to have a stroke; the patient has to understand that it is avoidable, and you must take the medication.’

Professor John Camm explains why adherence to anticoagulation is crucial in patients with AF and how this can be improved
Patient knowledge and perspective of anticoagulation therapy was also highlighted during a session on shared decision making in AF in practice. Professor Laurent Fauchier (Tours, France) discussed how patients with a low CHA2DS2-VASc score typically do not want to start oral anticoagulation and how it is essential to discuss with patients in simple language why lifelong oral anticoagulation is usually recommended. Furthermore, Inga Drossart (Brussels, Belgium), a member of the ESC Patient Forum, gave a personal account on how building rapport, discussing the patient’s values and preferences, and the development of a shared, adaptable plan that considers both the patient and physician perspective provides the most effective care.
Summary
Earlier detection of AF enables earlier initiation of anticoagulants for stroke prevention. Based on their relative effectiveness, safety and convenience across patient populations, and in clinical practice, NOACs are now recommended as the first line therapy for oral anticoagulation in eligible patients.1 NOACs can only confer these benefits, however, if patients will take their medication. Therefore, guidelines now place importance on physicians involving their patients in the management of their AF, and clearly explaining the importance of sticking to their treatment.1
The presentations from the congress are available on-demand via ESC 365.
References
- Hindricks G, Potpara T, Dagres N et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J 2021;42:373–498. Return to content
- Svennberg E, Friberg L, Frykman V et al. Clinical outcomes in systematic screening for atrial fibrillation (STROKESTOP): a multicentre, parallel group, unmasked, randomised controlled trial. Lancet 2021;398:1498–1506. Return to content
- Gibson CM, Mehran R, Bode C et al. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med 2016;375:2423–2434. Return to content
- Zeymer U, Tölg R, Hambrecht R et al. Use, safety and efficacy of rivaroxaban in patients with atrial fibrillation undergoing PCI – Results of the prospective RIVA-PCI registry. Deutsche Gesellschaft für Kardiologie Annual Congress. Mannheim, Germany, 7–10 April 2021. Abstract 37. Available at: https://dgk.org/kongress_programme/ht2021/abstracts/aP753.html?q=zeymer [accessed 7 April 2022]. Zeymer U, Tölg R, Hambrecht R et al. Use, safety and efficacy of rivaroxaban in patients with atrial fibrillation undergoing PCI – Results of the prospective RIVA-PCI registry. Deutsche Gesellschaft für Kardiologie Annual Congress. Mannheim, Germany, 7–10 April 2021. Abstract 37. Available at: https://dgk.org/kongress_programme/ht2021/abstracts/aP753.html?q=zeymer [accessed 7 April 2022]. Return to content
- Collet JP, Thiele H, Barbato E et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289–1367. Return to content





