ESVM 2019 Congress Highlights
Congress overview
For their fifth annual meeting, the European Society of Vascular Medicine (ESVM) met on 10–12 October 2019 in Ljubljana, Slovenia, for a joint congress with the European Chapter of the International Union of Angiology, the Central European Vascular Forum, and the Slovenian Society for Vascular Diseases. The scientific programme covered the full spectrum of vascular diseases and included several presentations and discussions on the topic of peripheral artery disease (PAD).

Understanding the burden of peripheral artery disease
A recurring theme across the scientific sessions at ESVM was the huge burden associated with PAD. However, as noted by Professor Lucia Mazzolai (Lausanne, Switzerland) in a session on the epidemiology of lower-extremity PAD in Europe, the precise scale of this burden may be underestimated because there are only limited country-level studies available.
The results of one national study, known as PID-PAB, were presented by Professor Aleš Blinc (Ljubljana, Slovenia), who was also a member of the ESVM 2019 local organizing committee. The study had evaluated outcomes in patients with PAD in Slovenia who were treated in accordance with European guidelines. Despite receiving a very high standard of therapy, patients remained at high continuing risk of ischaemic events and had high mortality rates compared with patients without PAD.1
Professor Blinc was also Chair of the Bayer-sponsored symposium ‘Improving Outcomes in Patients with Lower Extremity PAD in the New Era of Dual Pathway Inhibition’ where he explained, for patients with lower-extremity arterial thrombosis, that in-hospital mortality remains high despite revascularization, thus there is an urgent need for new therapies to improve outcomes in these patients.2

Mortality in patients hospitalized with lower-extremity atherothrombosis has remained high despite revascularization2
From trials to guidelines to clinical practice
Following Professor Blinc’s summary of the burden of PAD, ESVM past president Professor Marianne Brodmann (Graz, Austria) summarized the results of the COMPASS trial explaining that ‘with these data, we have for the first time something that can cause a shift in how we treat PAD’. Professor Brodmann drew attention to the subanalysis of major adverse limb events (MALE; severe limb ischaemia leading to an intervention or major vascular amputation) in the COMPASS trial, which showed that rivaroxaban vascular dose 2.5 mg twice daily (bid) plus aspirin reduced the incidence of MALE by 46% compared with aspirin alone.3
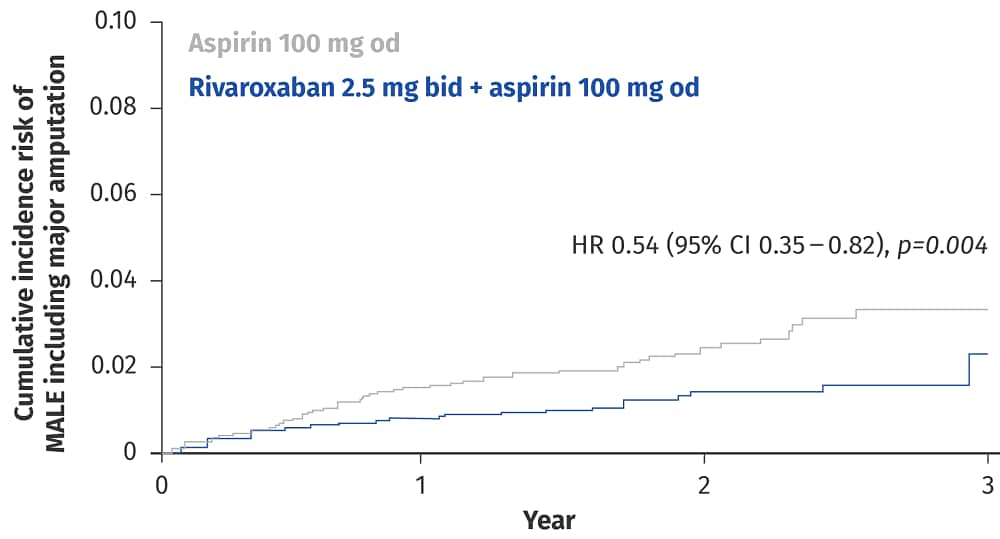
Rivaroxaban 2.5 mg bid plus aspirin is associated with a significant reduction in the risk of MALE compared with aspirin alone3
CI, confidence interval; HR, hazard ratio; od, once daily
To provide guidance on the use of rivaroxaban vascular dose plus aspirin, Professor Sigrid Nikol (Hamburg, Germany) and ESVM President Professor Jill Belch (Dundee, UK) presented some real-life patient cases in which they had treated patients with this regimen.
Professor Nikol’s patient had a complicated, severe case of polyvascular disease with a history of multiple vascular interventions, coronary artery disease, stage III chronic kidney disease and multiple risk factors such as smoking. With a high risk of major adverse cardiovascular events and MALE associated with their co-morbidities, the patient stood to benefit greatly from the protection offered by the rivaroxaban vascular dose plus aspirin regimen.

Professor Jill Belch discusses the treatment of a patient with PAD
The patient in the case presented by Professor Belch also had polyvascular disease. Consistent with the underdiagnosis of PAD discussed widely at this meeting, the patient’s intermittent claudication had initially been dismissed by their general practitioner as age-related back pain. However, the patient later presented with leg pain at rest and was diagnosed with chronic limb ischaemia by a vascular surgeon. Despite receiving optimized risk factor management, the patient’s unacceptably high continuing risk of further ischaemic events meant that they were started on rivaroxaban vascular dose plus aspirin.
Professor Belch also introduced chapter 5 of the new ESVM guidelines for the management of PAD. The guidelines’ application of the COMPASS data was of particular interest in relation to the patient cases described at the meeting:
‘Based on the results of the COMPASS trial, the combined therapy of ASA 100 mg/d and rivaroxaban 2 × 2.5 mg/d should be considered in PAD patients without a high risk of bleeding, or other contraindications. (Evidence level B, Recommendation class IIa)’
What’s new in the ESVM guidelines?
Chapter 5 of the new ESVM guidelines can be read here.
For more information, watch the following videos:
PP-XAR-ALL-1528-2
PP-XAR-ALL-1561-1
“[With the] COMPASS study [...] we show [for] the first time that we re able to save limbs.”
Professor Marianne Bromann
Summary
It is becoming increasingly clear that the new therapeutic option provided by the rivaroxaban vascular dose plus aspirin regimen has the potential to revolutionize the treatment of PAD and protect these patients from devastating events such as stroke, myocardial infarction and limb loss. Although positive trial results generate excitement, it is only through practical experience and expert guidance that practice can change.
By acknowledging the impressive results of the COMPASS trial, the new ESVM guidelines join the ESC guidelines on chronic coronary syndromes, the ESC/EASD guidelines on diabetes management, and the Global Vascular Guidelines for chronic limb-threatening ischaemia, by providing guidance on those patients who stand to benefit from vascular dose rivaroxaban 2.5 mg bid plus aspirin.4-6 As Professor Brodmann said in her closing remarks of the symposium, ‘PAD is a deadly disease and we need to do everything we can to improve outcomes for our patients’.

The symposium panel discussing the treatment of PAD
Perspectives on venous thromboembolism
As a vascular medicine congress, ESVM saw not only discussion of arterial conditions but also ample time was given to discussing the treatment and prevention of venous disorders. In line with recent ESC guidelines for the management of acute pulmonary embolism, Professor Russell Hull (Calgary, Canada) summarized a recent review, explaining that it is no longer sufficient to categorize venous thromboembolism as provoked or unprovoked, and that the decision to extend anticoagulation should be based on the likelihood of recurrence in an individual patient.7,8 Another important subject for discussion was the use of non-vitamin K antagonist oral anticoagulants to treat cancer-associated thrombosis, with Professor Cecilia Becattini (Perugia, Italy) showing the evidence behind the recent guidance from the ESC that rivaroxaban and edoxaban should be considered as alternatives to low molecular weight heparin in patients with pulmonary embolism and active cancer that is not gastrointestinal.8
References
- Blinc A, Kozak M, Sabovic M et al. Survival and event-free survival of patients with peripheral arterial disease undergoing prevention of cardiovascular disease. Int Angiol 2017;36:216–227. Return to content
- Korabathina R, Weintraub AR, Price LL et al. Twenty-year analysis of trends in the incidence and in-hospital mortality for lower-extremity arterial thromboembolism. Circulation 2013;128:115–121. Return to content
- Anand SS, Caron F, Eikelboom JW et al. Major adverse limb events and mortality in patients with peripheral artery disease: the COMPASS trial. J Am Coll Cardiol 2018;71:2306–2315. Return to content
- Knuuti J, et al. Eur Heart J. 2019;ehz425. doi:10.1093/eurheartj/ehz425. Knuuti J, et al. Eur Heart J. 2019;ehz425. doi:10.1093/eurheartj/ehz425. Return to content
- Cosentino F, et al. Eur Heart J. 2019;ehz486. doi:10.1093/eurheartj/ehz486. Cosentino F, et al. Eur Heart J. 2019;ehz486. doi:10.1093/eurheartj/ehz486. Return to content
- Conte MS, Bradbury AW, Kolh P et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg 2019;69:3S–125S.e140. Return to content
- Albertsen IE, Piazza G, Goldhaber SZ. Let's stop dichotomizing venous thromboembolism as provoked or unprovoked. Circulation 2018;138:2591–2593. Return to content
- Konstantinides SV, Meyer G, Becattini C et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J 2019: doi:10.1093/eurheartj/ehz405. Return to content


