ESC Heart Failure Conference Highlights from Bayer
25-28 May 2019
Conference Overview
Around 5400 participants from 105 countries made their way to Athens, Greece for the 6th annual Heart Failure Congress, organized by the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). The conference brings together a broad range of specialists and non-specialists to discuss every aspect of heart failure (HF), from acute to chronic and from prevention to treatment. Reflecting the broad range of participants and topics, the programme featured a mix of symposia, practical tutorials, ‘Guidelines in Daily Practice’ sessions, debate sessions and more.

The Heat Failure Congress was held in Athens, Greece
The Heart, Kidneys and Brain: Three Pieces of the Same Puzzle?
We often think of HF, diabetes, kidney disease and atrial fibrillation as separate diseases, but in reality these conditions are seldom seen in isolation. The Bayer-sponsored symposium at the Heart Failure Congress was one of several to focus on the interactions between these conditions, the impact on patient treatment and outcomes, and the future of cardiology. Professor Martin Cowie (London, UK) opened the symposium by highlighting just a few of the many pathophysiological links between these conditions. HF specialists see patients with co-morbidities every day, so they know the importance of holistic management.
“Only by considering all the risks to the patient’s health can we protect them not just from heart failure progression, but also from events such as renal failure, stroke or myocardial infarction.”
(Professor Martin Cowie, Heart failure specialist)

Professor Cowie highlights some of the interlinked conditions affecting patients with heart failure
Managing Atherothrombotic Disease
In 2017, the COMPASS trial was stopped early because of a significant reduction in major adverse cardiovascular events (MACE), defined as stroke, myocardial infarction or cardiovascular death, in patients with chronic coronary or peripheral artery disease receiving rivaroxaban vascular dose 2.5 mg twice daily (bid) plus aspirin compared with those receiving aspirin alone.1 Dr Kelley Branch (Seattle, USA) presented his latest data on the population of patients in COMPASS with concomitant chronic HF. The higher absolute cardiovascular risk in these patients translated into a greater absolute benefit with rivaroxaban vascular dose plus aspirin, with a 34% relative risk reduction and a 2.4% absolute risk reduction in MACE compared with aspirin alone over the course of the trial.2,3 No difference in major bleeding risk was observed between the two regimens.
“These patients are not stable – they have a chronic disease and our job is to slow down the progression to prevent cardiovascular events”
(Dr Kelley Branch, HF specialist)

Risk of cardiovascular death, stroke or myocardial infarction in patients with or without HF in the COMPASS trial. ARR, absolute risk reduction; CI, confidence interval; CV, cardiovascular; HR, hazard ratio; MI, myocardial infarction; NNT2y, number needed to treat over 2 years
Risk of cardiovascular death, stroke or myocardial infarction in patients with or without HF in the COMPASS trial. ARR, absolute risk reduction; CI, confidence interval; CV, cardiovascular; HR, hazard ratio; MI, myocardial infarction; NNT2y, number needed to treat over 2 years
This subanalysis, soon to be published in Circulation, additionally investigated the effect of left ventricular ejection fraction on outcomes. A 32% reduction in the risk of MACE was observed in patients with an ejection fraction 40% or above, and a numerically lower 18% risk reduction was observed in those with an ejection fraction between 30 and 40% due to higher cardiovascular death rates (patients with an ejection fraction below 30% were excluded from the trial).2 These results were consistent with the MACE reduction in the overall trial. No clinical trial specifically in patients with preserved ejection fraction has demonstrated a reduction in mortality and morbidity,4 so these results may offer a new treatment opportunity for a subset of these hard-to-treat patients.
A video of Dr Kelley Branch discussing the COMPASS results in patients with chronic HF can be found online at Tools and Resources
BREAKING NEWS
Clinical Practice Update: Patients with CAD and Heart Failure
The 2019 Heart Failure congress saw a new clinical practice update issued by the HFA, taking into consideration the wealth of recent data. Among several important guidance updates, the document stated that “For ambulatory patients with CAD and HF in NYHA class I/II with an ejection fraction >30%, addition of rivaroxaban 2.5 mg to background treatment with aspirin may be considered in order to reduce the risk of stroke and CV death.”, reflecting the COMPASS data. The authors conclude “it appears that for patients with CAD rivaroxaban 2.5 mg twice daily in addition to low-dose aspirin reduces the risk of vascular events in patients without HF and with mild HF. However, for patients with advanced HF, myocardial dysfunction and congestion rather than vascular events determine outcome.” They note however that stopping of pre-existing rivaroxaban therapy in patients who develop NYHA class III/IV symptoms cannot be recommended as there is no related evidence.
Protecting Patients Against the Triple Threat of Atrial Fibrillation, Heart Failure and Kidney Disease
Like HF, atrial fibrillation (AF) is a condition for which comorbidities are the rule, not the exception. Professor Hendrik Bonnemeier (Kiel, Germany), discussed the intersection between AF, HF, kidney disease and diabetes, and the treatment considerations necessary in managing the cardiovascular patient with multiple comorbidities.
Considering that AF and renal dysfunction are both strongly age-related, it should be no surprise that the two conditions frequently coincide. The combination is associated with a poor prognosis, with significantly higher rates of both stroke and bleeding in patients with concomitant AF and non-end-stage kidney disease compared with AF alone. This high stroke risk underlines the importance of anticoagulation in these patients; however, reliable protection consists of both efficacy and safety, and safety encompasses more than bleeding. Traditional vitamin K antagonist (VKA) oral anticoagulants have been linked to a decline in renal function over time, perhaps due to an increase in calcification of the renal blood vessels, which has made many physicians reluctant to use these agents in patients with renal impairment.
Professor Bonnemeier discussed recent data collected from daily clinical practice suggesting that some non-VKA oral anticoagulants (NOACs) may be associated with better preservation of renal function over time than VKAs in patients with AF. In particular, results from the RELOADeD real-world evidence study recently presented at the conference of the German Society of Cardiology (DGK) indicated that
Rivaroxaban was associated with a significant reduction in the development of end-stage renal disease or dialysis and a tendency towards a reduction in acute kidney injury compared with the VKA phenprocoumon.5
The study included over 17,000 patients from a large German insurance claims database, making it the largest to date to compare renal outcomes in patients receiving NOACs and VKAs.

Renal outcomes with rivaroxaban versus warfarin in the RELOADeD study5
No ‘One-Size-Fits-All’ Solution for Atrial Fibrillation and Heart Failure
It’s no surprise that AF and HF frequently coincide: they share risk factors, pathophysiology and even some symptoms. In a session held jointly with the European Heart Rhythm Association (EHRA), a panel of experts discussed the optimal treatment for these high-risk individuals, with the primary focus on whether to employ pharmacological rate/rhythm control approaches or to perform catheter ablation. The panel agreed that there can be no ‘one-size-fits-all’ approach in this population, and patient selection is therefore key to successful outcomes. A joint HFA-EHRA position paper on the topic is currently in development.
The HFA Clinical Practice Update is available online at:
https://onlinelibrary.wiley.com/doi/epdf/10.1002/ejhf.1531
Looking to a Digital Future
Professor Cowie also provided a look to the future, focusing on the power of digital solutions to improve outcomes in HF. Digital health solutions have long been described as the future of healthcare – whether in the shape of wearable or implanted monitors, apps to provide on-the-go access to medical advice, or even robots to enable remote diagnosis of patients. But can they live up to this promise, or is it just hype?
“This is a complex issue. Technology may help us – but where does our responsibility start, and where does it end?”
(Professor Martin Cowie, Digital Health Committee chair)
While researchers seek to establish the benefits of digital health solutions, several challenges to their implementation remain. The ESC Working Group on eCardiology published a position paper earlier this year looking at how these challenges can be overcome, and the first digital summit will be held this October in Tallinn, Estonia to discuss how digital health is disrupting the usual way in which patients and healthcare professionals interact.
For information and registration for the ESC Digital Summit 2019, go to
https://www.escardio.org/Congresses-&-Events/ESC-Digital-Summit
The Heart–Kidney Connection
Despite numerous therapeutic advances over the past decades, patients with HF remain at high risk of MACE and HF hospitalization. Professor Carolyn Lam (Singapore) looked at some of the newest therapeutic strategies on the horizon, focusing particularly on the intersection between HF and kidney disease: a topic she described as “the final frontier” in HF research.
Kidney disease is common among patients with HF, and a body of evidence has demonstrated that poor renal function correlates with poor outcomes in HF. Yet despite this link, patients with severe kidney disease have been excluded from almost every randomized clinical trial underpinning standard therapy for HF. The resulting knowledge gap has become increasingly apparent as research has demonstrated that many of the same pathophysiological processes underlie both HF and renal dysfunction.
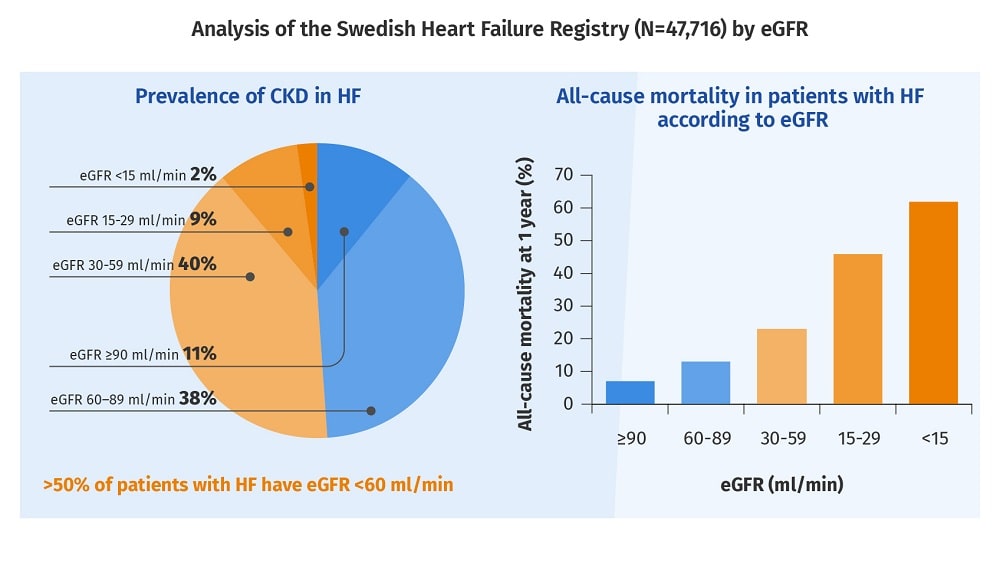
Kidney disease is common among patients with HF and is associated with a poor prognosis. CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate, HF, heart failure
Professor Lam described four such processes: haemodynamic changes leading to glomerular hypertension; neurohormonal changes and activation of the renin–angiotensin system; fibrosis; and microvascular dysfunction. New therapies aiming to address each of these pathways are already being examined in clinical trials, including FIDELIO (NCT02540993), FIGARO (NCT02545049), VICTORIA (NCT02861534) and VITALITY (NCT03547583).
Putting Patients First
In a session on patient and family engagement, the topic of patient centricity was discussed at every stage of the journey from clinical trials to guidelines. Even the ESC is taking this up, with a range of initiatives designed to improve engagement with both patients and their caregivers. The new ESC ‘patient forum’ is a panel of 24 patients who are supporting the ESC by providing their feedback on materials for patients, contributing to the ESC core curriculum for the cardiologist, speaking at conferences and contributing to the development of guidelines. This shift in thinking will have a major impact on the HF landscape of the future.
“Patients are the experts on what it means to experience heart disease”
(Professor Donna Fitzsimons, ESC board member and lead for patient engagement)
For more information on the ESC patient forum, visit www.escardio.org/patients
Another Clinical Cross-Talk: Managing the Patient with Acute Heart Failure and Pulmonary Embolism
In an interactive case-based discussion, Dr Ioulia Grapsa (London, UK) presented the case of a complex patient who presented to her hospital in acute cardiogenic shock, caused by a massive pulmonary embolism (PE) leading to acute HF. In an acute patient such as this, rapid diagnosis and treatment of the acute PE are essential. Two experts provided their perspectives, followed by a panel discussion addressing both acute and chronic aspects of the patient’s care. Once the patient had stabilized, most panel members agreed that a NOAC would be most appropriate for long-term management in high-risk cases.

Participants at the ESC-HF congress
Further Information
Learn more about the prevention of atherothormbotics events in patients with CAD
The 7th annual congress of the ESC Heart Failure Association will take place on the 23–26 May 2020 in Barcelona, Spain.
References
- Eikelboom JW et al. N Engl J Med 2017;377:1319–1330. Return to content
- Branch KR et al. Circulation 2019;[in press]. Return to content
- Branch K. European Society of Cardiology Heart Failure Congress. Vienna, Austria, 26–29 May 2018, Abstract 1591. Return to content
- Roh J et al. Circ Res 2017;120:1243–1245. Return to content
- Bonnemeier H. German Cardiology Society. Mannheim, Germany, 24–27 April 2019, Oral V1126. Return to content


