Limb events in CAD patients with PAD: The consequences can be severe
Patient case: CV risk in polyvascular disease
Consider the following clinical situation:
- Henry presents to primary care with a leg wound that has not healed. He is 54 years old and has a history of stable CAD, diagnosed after he presented with stable angina
- Since the diagnosis of angina, he has been receiving a beta blocker, aspirin and a statin, along with an ACE inhibitor to treat his hypertension and a nitrate to treat angina attacks
- The clinician suspects that Henry might have PAD, and after measuring his ABI as 0.73, their suspicion is confirmed

Henry has peripheral artery disease
How does this new diagnosis affect Henry’s risk of major adverse CV events?
Registry data have shown that patients with CAD and concomitant PAD are twice as likely to die from a CV cause as patients with CAD alone (1-year risk of CV death: CAD alone, 1.58%; CAD + PAD, 3.23%).1
What measures should be implemented to reduce his risk of CV events?
Limb events are associated with severe, life-changing outcomes
Half of patients diagnosed with PAD undergo a revascularization procedure to restore blood flow to the limb and relieve symptoms.2 However, only one-quarter of these patients are reported to be free of symptoms after 1 year. Within 1 year of a revascularization procedure, more than half of patients will either have died or have survived after having undergone amputation.

One year after revascularization, the majority of patients will have died or undergone amputation
The poor prognosis associated with a revascularization procedure shows that
a patient in whom atherosclerosis has progressed enough to require revascularization continues to be at high risk of another serious event.
A subanalysis of the COMPASS randomized controlled trial also investigated the risks associated with limb events in 6391 patients with lower extremity PAD.3 The trial compared the prognosis of patients who had experienced a major adverse limb event (MALE), defined as acute or chronic limb ischaemia, including all major vascular amputations.
Compared with those patients who did not experience a MALE, patients who did were almost 200 times more likely to undergo a subsequent amputation, seven times more likely to be hospitalized and three times more likely to die based on 1-year cumulative risk.
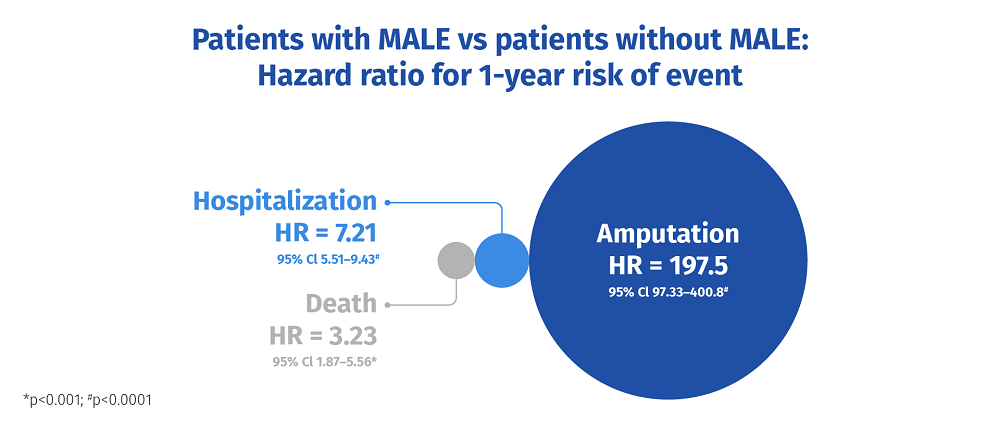
COMPASS: One-year risk of events was higher in patients who experienced a MALE than in patients who did not (N=6519)
Treatment choice should address the risk of major adverse limb events
Because of their profound negative effect on quality of life, all limb events – but especially amputations – are greatly feared by patients, and the risk of MALE should therefore be considered when choosing an antithrombotic regimen. For this reason, the COMPASS subanalysis also evaluated whether rivaroxaban 2.5 mg bid plus aspirin affected the risk of MALE compared with aspirin alone.
Patients in the study were already receiving a good standard of secondary prevention
Treatments:
- Lipid-lowering agents were used by 82.3% of patients
- An ACE inhibitor or ARB was used by 69.7% of patients
As shown in the figure, rivaroxaban 2.5 mg bid significantly reduced the risk of MALE by 43% (ARR, 1.1%) compared with aspirin alone and was also associated with significant reductions in the risk of amputation and vascular interventions.

COMPASS: Rivaroxaban 2.5 mg bid plus aspirin reduced the risk of MALE, amputation and vascular intervention compared with aspirin alone
Conclusion
Rivaroxaban 2.5 mg bid plus aspirin offers a new treatment option for patients with PAD and can reduce the risk of life-changing events. As Professor Sonia Anand explains in the video below,
“This is a substantial advance for patients with PAD for whom, until now, the standard of care has been aspirin only. Treatment with rivaroxaban and aspirin should be initiated in symptomatic PAD patients in order to prevent MALE, thereby reducing the future risk of both death and amputation”.
PP-XAR-ALL-0786-2
References
- Steg PG, et al. JAMA. 2007;297:1197-1206. Return to content
- Norgren L, Hiatt WR, Dormandy JA et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 2007;45:S5–S67. Return to content
- Anand SS, Caron F, Eikelboom JW et al. Major adverse limb events and mortality in patients with peripheral artery disease: the COMPASS trial. J Am Coll Cardiol 2018;71:2306–2315. Return to content


